Tous droits réservés © NeurOreille (loi sur la propriété intellectuelle 85-660 du 3 juillet 1985). Ce produit ne peut être copié ou utilisé dans un but lucratif.
Tomorrow, technological advances will undoubtedly give rise to improved prosthetic devices (hearing aids and implant), which will remain, in the short-term at least, the major mode of rehabilitation.
However, one can predict the development of local pharmacology (across the eardrum) to protect hair cells and neurons, and to treat tinnitus.
And after that? Regeneration? Cell-based or gene therapies?
Hair cells regeneration ?
Currently, and probably for years to come, regeneration of human hair cells remains a dream... Inaccessible? Who knows? Either way, research teams across the world are on the case, encouraged by initial studies into the inner ear of birds...
A large majority of acquired hearing loss is linked to hair cell death. Schematically, we pass through the three stages shown in the animation below: normal organ of Corti/ damage and disappearance of hair cells and their supporting cells/ a single layer of non-specific cells.
S. Blatrix, from J. Stone
Hope for regenerative therapies was first born in the '90s when it was discovered that the inner ear of birds can regenerate hair cells that have been damaged by drugs or noise trauma and reconnect them to the brain! Many research groups around the world have since been trying to reproduce this regeneration in the mammalian cochlea. No luck so far: our hair cells are still not regenerating !
Research continues in two directions. One (A) is to manage to 'wake up' some dormant stem cells that can be found in the adult cochlea.
The other (B) is to try to graft embryonic stem cells into the cochlea, then help them to differentiate into hair cells to take the place of those that are missing.
In both of these cases, we would then need to help them to connect to the brain.
The challenge is great, and we cannot, at this stage, tell whether they will work, nor give a date of a potential therapy using this technique.
Other uses for cell and gene therapies ?
In the meantime, one can expect a closer use of cell and gene therapies.
Our knowledge of which genes are involved in various types of hearing loss is constantly improving. It is now possible to imagine that future therapies may allow the correction of faulty genes to enable the auditory system to work properly again.
Towards local and specific pharmacology.
We have seen that the large majority of hearing problems are caused by environmental trauma (loud noise, ototoxic drugs...). To achieve good results with hearing aids and implants, it is crucial that cells survive. Research is already well under way.
We now know more and more about the biological and molecular mechanisms involved in cell death in the inner ear. We can therefore target protection treatments at sensory cells or cochlear neurons or increase their resistance to damage.
Currently, the primary obstacle to human clinical trials is the potential side effects of these therapeutic molecules if they are administered non-specifically.
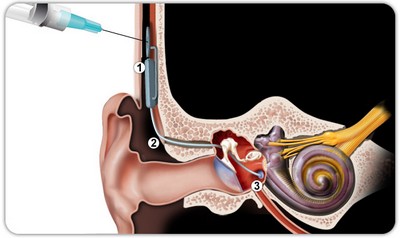
Local administration of these effective molecules at the round window is possible (as in the drawing below) !
| S. Blatrix, from J-L. Puel |
Mini-pump implant
|
The commercialisation of a number of delivery systems (catheter, syringe, etc...) allows us to conceptualise numerous promising therapies which could become acute treatments. Such devices are already used to treat dizziness!
More sophisticated methods such as the implantation of a pump that can be recharged through the skin can now be imagined. These pumps could be coupled with cochlear implants, with an aim to keep as many neurons as possible alive, improving the performance of the implant.
Showing that cell degeneration can be stopped in patients with cochlear implants will allow this type of pharmacological approach to spread to other pathologies, such as presbycusis, ...
 Français
Français
 English
English
 Español
Español
 Português
Português


Facebook Twitter Google+